Understanding Cirrhosis of the Liver
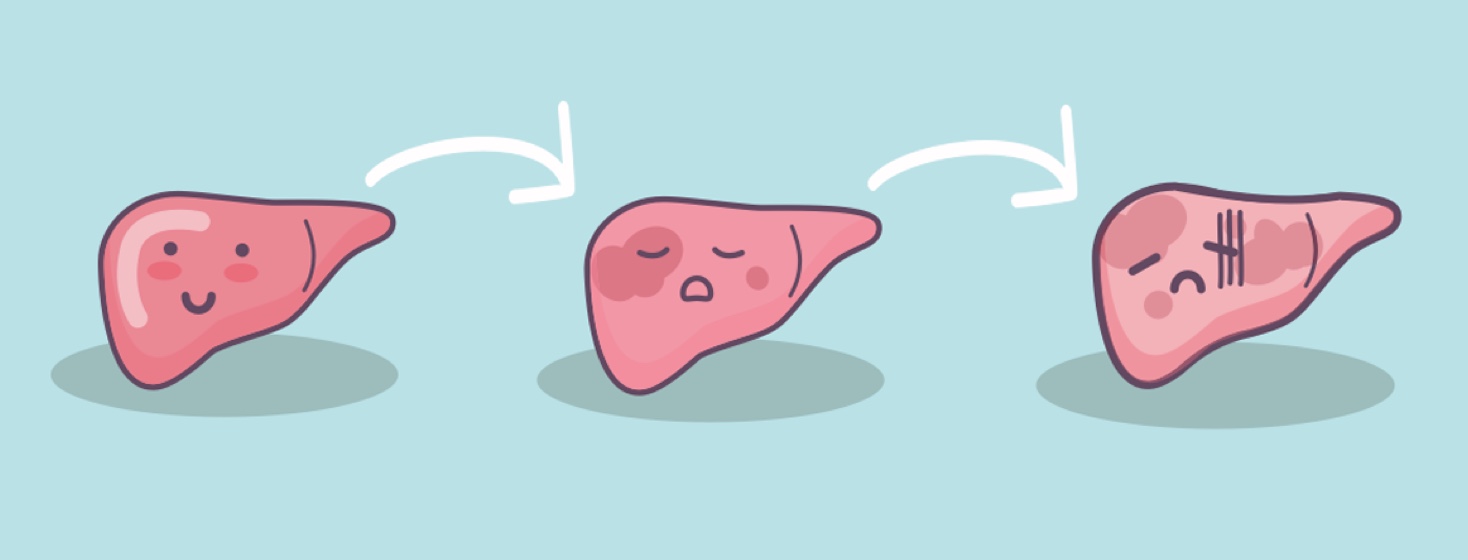
Cirrhosis of the liver is a severe condition in which there is permanent scarring and damage to the liver. As cirrhosis worsens, the liver becomes more damaged. This can lead to liver failure.1,2
What is cirrhosis of the liver?
Cirrhosis occurs when healthy liver tissue is gradually replaced by scar tissue. This gradual scarring is known as fibrosis. When fibrosis gets to an advanced stage that cannot be reversed, it becomes known as cirrhosis.1,2
How common is cirrhosis?
About 1 in 400 people in the United States are reported to have cirrhosis. But experts believe this number should be higher. That is because many people who are in the early stages of cirrhosis are not diagnosed.2
What are the causes and risk factors for cirrhosis?
Cirrhosis has various causes, such as:1-4
- Alcohol-associated liver disease
- Hepatitis C
- Hepatitis B
- Buildup of fat in the liver, known as nonalcoholic fatty liver disease (NAFLD)
- An advanced form of NAFLD that causes inflammation to the liver, known as nonalcoholic steatohepatitis (NASH)
Other things that increase your risk of cirrhosis include:2
- Being overweight or having obesity
- Having type 2 diabetes
- Being over 40 years old
- Being male
How does cirrhosis affect the liver?
In cirrhosis, the scar tissue that forms prevents crucial blood flow through the liver. The blood that enters the liver makes it possible for the liver to perform its many functions.1
The liver is a vital organ. It removes harmful substances from the body, produces bile for digestion, and stores essential nutrients. As cirrhosis progresses, the liver has a harder time with these jobs. This can lead to a range of health issues.1
When a person has cirrhosis:1,3
- The liver cannot filter out toxins. This leads to a buildup of toxins in the body. And that can lead to symptoms like confusion and fatigue.
- The liver makes less bile, which affects the digestion and the body’s ability to absorb key nutrients.
- Blood flow to the liver is blocked. Blood pressure increases in the portal vein, a main source of blood to the liver. This causes enlarged veins and can lead to severe bleeding.
Over time, reduced liver function can result in:1,3
- Portal hypertension – increased blood pressure in the portal vein
- Liver failure – the liver is unable to function properly
- Liver cancer – cancer cells grow in the liver
What are the symptoms of cirrhosis?
In the earliest stages of cirrhosis, there may be no noticeable symptoms. This is also known as compensated cirrhosis. The liver is a resilient organ. So, symptoms may not be noticeable until cirrhosis becomes more advanced.1,4
Early symptoms of cirrhosis may include:4
- Fatigue
- Itchy skin
- Muscle cramping
- Weakness
- Loss of appetite
- Unexplained weight loss
As the disease progresses, more severe symptoms can develop (decompensated cirrhosis). These symptoms include:1,4
- Easy bruising and bleeding
- Confusion, difficulty thinking clearly, memory loss, or mood changes (hepatic encephalopathy)
- Dark urine
- Yellowing of the skin and eyes (jaundice)
- Swelling in the legs, ankles, and feet (edema)
- Swelling of the abdomen, due to fluid buildup (ascites)
- Enlarged veins in the esophagus or stomach (varices)
What is the prognosis for people with cirrhosis?
For those with cirrhosis, outcomes vary based on the cause and severity of the disease. About 20 percent of people with NASH will go on to develop cirrhosis over time.1,3
How is cirrhosis diagnosed?
Cirrhosis is diagnosed through a combination of:5
- Medical history
- Physical exam
- Liver enzyme tests
- Complete blood count
- Imaging tests, like ultrasound, computed tomography (CT) scans, and magnetic resonance imaging (MRI)
- Liver biopsy
Physical exams may reveal signs like jaundice or an enlarged liver. Blood tests are used to assess liver function and detect markers of liver damage. Imaging provides detailed views of the liver's structure. A liver biopsy, where a small tissue sample is examined under a microscope, may be performed to confirm the diagnosis and determine the extent of cirrhosis.5
How is cirrhosis diagnosed and treated?
There is no cure for cirrhosis. But various treatments can help manage symptoms, slow down liver damage, and address underlying causes. Key treatment approaches include:1,6
- Lifestyle changes
- Medicines
- Monitoring and screening
- Managing complications
- Liver transplant
Lifestyle changes
Avoiding alcohol, eating a healthy diet, and maintaining a healthy weight are crucial for those with cirrhosis. If you have NAFLD or NASH, the first approach to improving the health of your liver is losing weight.6
Medicines
Depending on the cause of cirrhosis, medicines can help manage symptoms and underlying causes. For example, antiviral drugs can help treat hepatitis.6
But certain medicines can harm the liver. Talk with your doctor about whether any medicines you are taking are unsafe.6
Monitoring and screening
Regular monitoring and screening for liver function and complications are essential. This may include blood tests, imaging studies, and liver biopsies.6
Managing complications
There are many complications tied to cirrhosis. For example:6
- If you have portal hypertension or varices, doctors may prescribe medicines to lower high blood pressure.
- For edema, doctors may prescribe medicines to reduce swelling.
- For hepatic encephalopathy, you may be prescribed medicines that reduce the amount of toxins in the brain and help improve brain function.
Liver transplant
If cirrhosis has led to liver failure, a liver transplant is the only treatment option. This involves replacing the damaged liver with a healthy one from a donor. Transplants can greatly improve survival and quality of life for people who have advanced liver disease.6
Don’t delay treatment
Cirrhosis of the liver is serious. It is a chronic condition that requires treatment to improve outcomes and survival rates. While there is no cure for cirrhosis, lifestyle changes, medicines, regular monitoring, and – in severe cases – liver transplants can help manage the condition.1,6
Join the conversation